Lingo

Armchair Diagnosis
I will start out with a disclaimer: I am not a clinician. Not a psychologist, or a psychiatrist, or a licensed clinical social worker. I diagnosed an actor for my clinical psych final in undergrad and have watched far too many crime shows centered on forensic psychology, but otherwise have no qualifications. However, I am dedicating my life to understanding the brain and what happens to it during disease. I hope that in the spirit of looking at the past with new eyes you will tolerate some reckless speculation on my part, which will largely be based on diagnoses that historians and doctors have already proposed for the monarchs we will discuss in the months ahead.
Now to the man of the hour – Charles VI. There have been several theories of what caused his initial and subsequent breakdowns, but none seem as convincing to me as schizophrenia. To justify this, we will begin by looking at the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The first edition of the DSM was published in 1952 with the purpose of creating a reliable system to diagnose mental illness. The hope was that no matter what doctor a patient went to, they would leave with the same diagnosis. The DSM is flawed to be sure, but as far as the tools we have to codify and reliably diagnose mental illness, it’s the go-to for clinicians. Published in 2013, the DSM-5 breaks mental illnesses into different categories, and provides strict diagnostic criteria for each disorder.
Delusions and Disorganization
In the case of schizophrenia, we can distinguish between positive and negative symptoms. Positive symptoms are present during the “active” periods of disease and are probably what your mom was thinking of when she warned you against smoking pot in high school: delusions, hallucinations, speech that doesn’t make sense, and disorganized thoughts and actions. Negative symptoms crop up outside of those psychotic episodes and are things like lack of emotion, decreased speech, social withdrawal, and lack of interest or pleasure in normal activities (no you don’t have schizophrenia, you’re just in coronavirus quarantine). According to the DSM-5, for someone to be diagnosed with schizophrenia they would need to show a minimum of two symptoms for at least a month. One of these symptoms has to be a hallmark symptom of delusion, hallucination, or disordered speech. As you might guess would happen if you were suddenly hallucinating or consumed with paranoia, there also has to be evidence that the symptoms interfere with your job, relationships, or ability to care for yourself.

That brings us back to Charles. There were times when he thought he was made of glass (I’ll talk more about this in this month’s mini blog!), believed he was St. George, and was convinced he was being persecuted. Delusions – check. He sometimes “babbled nonsense.” Disordered speech – check. His fits of insanity were followed by periods where he just laid in bed, unable to do anything else, which is consistent with negative symptoms. While the duration of his first episode is unclear, historians report that as time went on Charles experienced more frequent and lengthy relapses. Modern studies of patients who have stopped taking their medications have found a similar pattern. They report that with each successive relapse a person experiences, they are less capable of recovering to their previous level of functioning. And I don’t think I have to convince you that Charles’ symptoms interfered with his ability to work. Handing the throne over to your rival country definitely won’t earn you an employee of the month certificate.
A couple of our readers guessed that Charles had bipolar disorder, and that’s a pretty good guess! In fact, these two disorders are often confused because of how “schizophrenic” and “bipolar” are used colloquially. Like schizophrenia, bipolar disorder, specifically bipolar I which is associated with impaired functioning, manifests in two distinct states. Bipolar patients experience periods of mania followed by depression. Some bipolar patients experience delusions or hallucinations, but in general these manic episodes are distinct from psychotic episodes in schizophrenia, and are characterized by increases in activity and talkativeness, decreased sleep, and an inflated ego. Bipolar periods of depression are also distinct from negative symptoms of schizophrenia, because they don’t necessitate the absence of activity. The historical sources describe Charles as being more erratic than manic, and the hallmark symptoms of delusions and disordered speech make schizophrenia a more plausible explanation to me.
I do want to take a moment to talk about the violence associated with Charles’ first psychotic episode (see Stefanie’s blog from last week). Mental illness is unpredictable, and thus those afflicted with it are often perceived as unpredictable and dangerous. While there is some relationship between schizophrenia and violence, especially during periods of positive symptoms, it is important to note that overall violence is not more common in those suffering from mental illness than the rest of the population. Therefore, we can’t use the fact that Charles killed several of his knights that day in the woods out of context to point to the fact that he may have been schizophrenic, or suggest that all schizophrenic people would kill their knights…if people still had knights, that is.
One of the less classical symptoms Charles had that I find interesting was his intermittent inability to recognize the faces of his family members. In 2016, a study by researchers at Harvard built off of many experiments reporting deficits in facial perception in schizophrenic patients. They recorded patients’ subjective performance on two different tasks. In the first, participants reported their level of everyday difficulty recognizing faces, which was a proxy for their application of facial information to social settings. In the other task, patients were evaluated on their performance on a task requiring them to pick out the face that matched a target image, indicating how well they are able to process visual information about faces. Unsurprisingly based on the previous research, the researchers found that individuals with schizophrenia scored worse on both measures compared to healthy controls. However, there was another important difference between the two groups. In controls, performance in one test tended to track with performance on the other. Essentially, their ability to process sensory facial information and apply that information to everyday life were related, as you might expect. But in schizophrenic patients, these two abilities seemed to be unrelated, meaning that the ability to actually perceive faces and then the social implications of that perception are distinct processes in this patient population. Basically, this suggests that regions of the brain that perform different functions related to facial recognition (in this case sensory perception and social application of this information) are not communicating with one another.
The overactive gardener
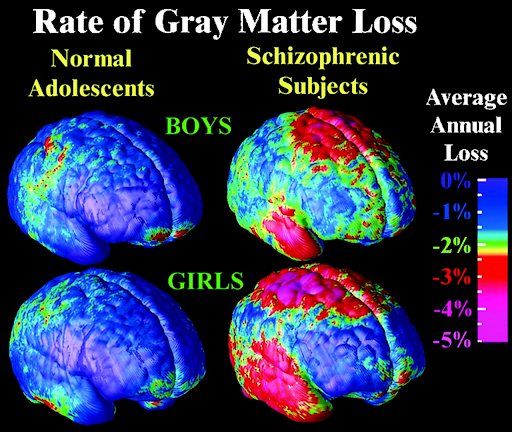
This brings us to the modern theory of the neurobiological basis of schizophrenia: a disease of altered neural connections. It was known for a long time that people with schizophrenia had fewer synapses, the connections between their neurons, and altered patterns of communication between brain areas, but it wasn’t until recently that scientists were able to understand why. A landmark paper published in January 2016 (by my scientific crush Dr. Beth Stevens) found that genetic variations associated with schizophrenia affect an immune-related protein called complement component 4 (C4). C4 is part of something called the complement pathway, which is a network of proteins of the immune system that identify junk or dangerous materials in the body and coordinate their removal. During some periods of development, the complement cascade is also important for getting rid of certain synapses. Complement proteins tag synapses that aren’t very active, meaning the neurons they are connecting aren’t talking to each other, and then these will get gobbled up by cells in a process called pruning. Imagine a gardener taking a pair of clippers to an overgrown tree so that the healthy branches can flourish.

Using a mouse test subject, the researchers in the Harvard paper found that C4 was able to trigger synapse elimination during a period of developmental pruning. Basically, this paper established a hypothesis (theory, not accepted dogma!) that changes to C4 in schizophrenia cause the gardener to get carried away, pruning too many synapses and ultimately impairing the brain’s ability to communicate, which could explain the disorganized thought patterns that characterize disease.
Your mom was right (kinda)
Okay, you might be thinking – I get it. It’s a genetic thing. Indeed, to some extent it is. Charles’ grandson Henry VI was also reported to experience periods of psychosis, suggesting that there was a genetic component. So why was Charles’ behavior normal until his early 20s if he always had this genetic defect? Well, that is actually the peak time of onset of schizophrenia in men, who are also more likely than women to develop the disease. This could be because brain regions that are affected in schizophrenia undergo a period of pruning in late adolescence and early adulthood, so C4 variations only manifest at this point. But it’s important to note that genetics cannot fully predict someone’s risk of having schizophrenia. Studies of affected families show that there is a complex inheritance pattern for schizophrenia, with close relatives often spared, and other disorders like bipolar disorder also present in the family tree. This indicates that genetics can predispose you to schizophrenia, but an environmental contribution is needed to develop the disease.

Going back to the lectures you got from your mom about the dangers of drugs, it has been shown that drug use during adolescence and young adulthood increase your risk of developing schizophrenia, as do exposures to infections before or soon after birth. Trauma and stress are also risk factors. I can’t answer why Charles’ brain came undone at the exact moment when it did. Did his mother catch the flu when she was pregnant with him? Did the stress of his position in power prime him for madness when he was attacked by a stranger? Were there subtle warning signs that failed to make it into the historical records? The comprehensive picture of what happened in the brain of Charles VI remains a secret of biology and nature. As exciting as the modern research is, there is still no complete picture of how schizophrenia develops or why.

Today schizophrenia requires lifelong treatment with antipsychotic drugs, often, but unfortunately not always, accompanied by therapy. Negative symptoms are less rarely targeted by therapeutics, and people with schizophrenia are much likelier to die prematurely, mostly due to a tragically high suicide rate. While there is much to be done in the realm of understanding and treating schizophrenia today, there was dramatically less knowledge and understanding in France in the 14th and 15th centuries. Instead of getting medication and therapy, Charles VI was believed to be possessed, a common interpretation of the symptoms at the time. For centuries, schizophrenic patients were misunderstood, forced to endure “treatments” such as exorcism and blood-letting, made victims of charlatans and mystics who promised to heal them, and later abandoned to asylums where they were out of sight and out of mind. Things likely would have turned out differently for Charles and France had they known what we know now. Next week, we’ll talk about just that: how did the effects of Charles’ mental illness reverberate across Europe and throughout history?
References
For historical sources, see references from last week’s post, “Charles VI: Game of Thrones”
Causes: Schizophrenia. (n.d.). Retrieved March 31, 2020, from https://www.nhs.uk/conditions/schizophrenia/causes/
Chen, Y., & Ekstrom, T. (2016). Perception of faces in schizophrenia: Subjective (self-report) vs. objective (psychophysics) assessments. Journal of Psychiatric Research, 76, 136–142. doi: 10.1016/j.jpsychires.2016.02.012
Emsley, R., Chiliza, B., Asmal, L., & Harvey, B. H. (2013). The nature of relapse in schizophrenia. BMC Psychiatry, 13(1). doi: 10.1186/1471-244x-13-50
Hurley, K. (n.d.). What is Schizophrenia? DSM-5 Schizophrenia Definition & Symptoms. Retrieved March 31, 2020, from https://www.psycom.net/schizophrenia-dsm-5-definition/
Pompili, M., & Fiorillo, A. (2015, July 23). Aggression and Impulsivity in Schizophrenia. Retrieved March 31, 2020, from https://www.psychiatrictimes.com/schizophrenia/aggression-and-impulsivity-schizophrenia
Sekar, A., Bialas, A. R., Rivera, H. D., Davis, A., Hammond, T. R., Kamitaki, N., … Mccarroll, S. A. (2016). Schizophrenia risk from complex variation of complement component 4. Nature, 530(7589), 177–183. doi: 10.1038/nature16549
Truschel, J. (2019, November 25). Bipolar Definition and DSM-5 Diagnostic Criteria. Retrieved April 9 , 2020, from https://www.psycom.net/bipolar-definition-dsm-5/
What is Schizophrenia? (n.d.). Retrieved March 31, 2020, from https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia

I have seen the affects of adolescent drug use on mental health/longer term brain disease. I definitely now of one case of schizophrenia most likely related to drug use. Tragic.
LikeLike
This was so informative and thoughtful! I appreciate your sensitivity to the false narrative that those with mental illness are more prone to violence than the rest of the population. Well done!
LikeLike
Another great post by the ULTC crew! I was unaware of the prosopagnosia findings in SCZ. Looking forward to our next adventure together! XD
LikeLike
Excellent. I really learned a lot in regards to neuro information and mental illness. Love this narrative. Good job ladies.
LikeLike